Intraocular
pressure (IOP) is one of the most important parameters in the diagnosis and
treatment of glaucoma1. Glaucoma has been established
as the second leading cause of blindness. The treatment of glaucoma
focuses mainly on lowering intraocular pressure (IOP). The target IOP is often set to a level 20% to 30% of
IOP reduction, and consequent large IOP reduction
beyond 30% or even 40% in cases of advanced glaucoma2. The different
methods of tonometery are: Goldman Applanation tonometery, Noncontact (air-puff)
tonometery, Perkins tonometery, Tonopen tonometery, Transpalpebral tonometery3.
Goldmann Applanation Tonometer is the method of choice in the optometric and ophthalmological clinical
settings. Based on Imbert-Fick principle, the Goldmann tonometer assesses the
intraocular pressure by measuring the force necessary to applanate a fixed area
of cornea3.
Air puff tonometry is based on the principle of Applanation,
the central part of cornea is flattened by a jet of air to measure the level of
IOP5. The main advantages of
non-contact tonometers are that they are non-invasive and thus comfortable for
the patient with a minimal risk of infection. The performance of non-contact
tonometery and the interpretation of results are easier than with Goldmann
tonometery. Therefore, IOP screening with non-contact tonometer can be
delegated by ophthalmic assistants3. The purpose of this study was to evaluate the
difference, if any, between IOP measurements taken by a Goldman Applanation Tonometer and those taken by an Air Puff tonometer
MATERIAL AND METHODS
From
April 2011 to September 2011 this comparative study was done, 286 patients between 10 to 72 years of age, both male and
females coming to eye OPD for refraction and ocular examination included.
A complete history was taken from the patients and a thorough ocular
examination was done on all selected patients. Patients who have corneal
opacity or disfigured cornea, corneal ulceration or inflammation,
conjunctivitis or ocular infection, corneal dystrophy, corneal degeneration,
keratoconus and pterygium were excluded.
Selected patients were explained and after informed consent; two readings of
intraocular pressure were taken by consultant Ophthalmologist with Goldmann
applanation tonometer (Haag – streit AT900) and Air puff tonometer (Keeler
PT100) each, between 8 am to 1 pm.
DATA ANALYSIS
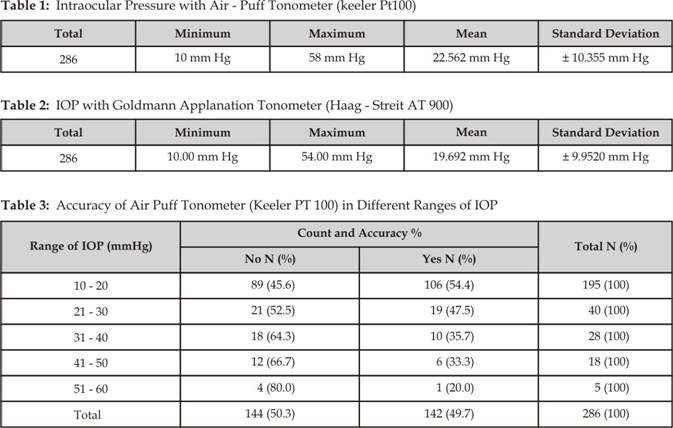
All
the data was computer based and SPSS version 10 was used for analysis. Mean and
standard deviation were computed for quantitative variables like age and
intraocular pressure readings. Frequencies and %age were computed for
categorical variables like sex, accuracy of air puff tonometer to measure IOP
in stratified ranges of IOP. Effect modifiers like age and genders were
controlled by stratification to observe the effect on outcome of accuracy of
air puff tonometer. All the data was presented in the form of tables 1, 2 and 3.
RESULTS
In
this study, 286 patients; 148 male and 138 female patients were included. The
mean ± SD age was 42.965 ± 16.304 years with range of age was 10 years to
maximum 72 years. The mean ± SD intraocular pressures were 19.692 ± 9.952 mm Hg
with Goldmann applanation tonometer as shown in table 2 and 22.562 ± 10.355 with air-puff tonometer as shown in
table 1. The range of measurement was 10 to 54
mm Hg with Goldmann applanation tonometer and 11 to 58 mm Hg with air-puff
tonometer.
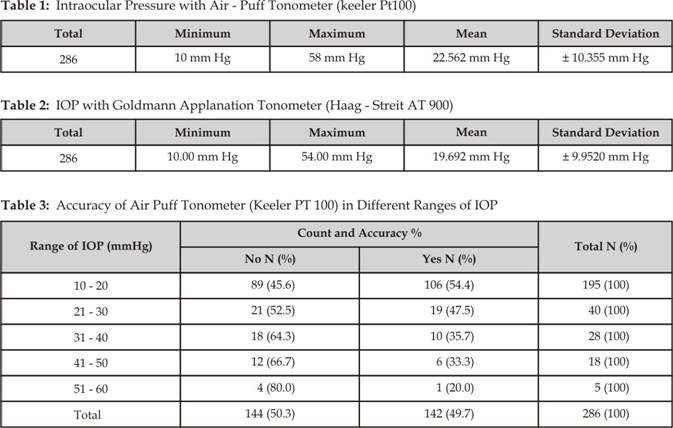
The
frequency of accuracy of air – puff tonometer within limit of ± 2 mm Hg from
Goldmann applanation tonometer was stratified over different ranges of
intraocular pressure as 10-20 mm Hg, 21 – 30 mm Hg, 31 – 40 mm Hg, 41 – 50 mm
Hg and 51 – 60 mm Hg. The overall frequency of accuracy of air-puff tonometer
was found to be 49.70%. This frequency of accuracy of air-puff tonometer was
different in different ranges of intraocular pressure as shown in table 3. It was most accurate 54.40% in normal range of intraocular
pressure i.e. 10 to 20 mm Hg and accuracy decreased with increasing range of
intraocular pressure. The accuracy was only 20% at 51 to 60 mm Hg range of
intraocular pressure. The frequency of accuracy of air-puff tonometer was
checked over different stratified ranges of age and found no specific pattern
of accuracy with age as shown in table 3.
DISCUSSION
More recently, the development of
noncontact tonometers has simplified IOP screening. Goldmann applanation
tonometer and Air Puff (i.e., noncontact) tonometers are the most
common devices for measuring IOP in daily practice. Air Puff tonometers
are easier to use and are more convenient, for both the patient and the
examiner, than GAT. The GAT is currently the most widely used instrument for measuring IOP4, and is considered the ‘gold standard’5.
Various studies have been done to assess the accuracy of air
puff tonometers in the past. A study conducted by Salim S et al6 to compare the measurements by the
portable, noncontact tonometer with Goldmann applanation tonometry. A
total of 98 eyes were examined for IOP. The results showed the mean ± SD
intraocular pressure measurements were 15.98 ± 5.48 mm Hg and 15.65 ± 4.26 mm Hg
for the PT100 and GAT, respectively. The range of measurements by GAT was
from 4 to 29 mm Hg and by PT100 was 7 to 33 mm Hg. The frequency of
measurements by the two tonometers that were in agreement by ≤ 3 mm Hg was 92.8%. The drawbacks of this study were limited
number of subjects and the most of the measurements were made in normal range
of IOP.
In this study
the air puff tonometer consistently overestimated IOP than Goldmann applanation
tonometer that was also shown in other studies7. In contrast some studies have shown that air
puff tonomaters returned lower values relative to goldmann tonometer. Yet the
other studies8 conclude that the air puff tonometers
overestimated at normal range of IOP and underestimated at high IOPs relative
to Goldmann applanation tonometer.
In
this study the accuracy of air puff tonometer was higher 54.40% in normal range
of IOP 10-20 mm Hg but the accuracy progressively decreased at higher ranges of
IOP.
CONCLUSION
Air puff
tonometer is quick, a non-contact method to measure intraocular pressure and is
useful for screening purposes but the measurements should be confirmed with
Goldmann applanation tonometer for accurate labelling of intraocular pressure.
Author’s Affiliation
Dr. Javied Ahmad
Medical Officer
Bahawal
Victoria Hospital, Bahawalpur
Dr. Muhammad Rizwan Khan
Medical Officer
Bahawal
Victoria Hospital, Bahawalpur
Dr. Muhammad Naeem Azhar
Ophthalmologist
LRBT
Free Eye Hospital, Lahore
Dr. Tariq Mahmood Arain
Associate Professor of
Ophthalmology
BVH
Bahawalpur
Dr. Zaheer-ud-Din Aqil Qazi
Chief Consultant
LRBT Free Eye Hospital, Lahore
REFERENCES
1.
Wells
AP, Garway-Heath
DF, Poostchi
A, Wong
T, Chan
KC, Sachdev
N. Corneal hysteresis but not corneal thickness
correlates with optic nerve surface compliance in glaucoma patients. Invest Ophthalmol Vis Sci. 2008;
49:
3262-8.
2.
Cheng JW,
Cheng SW, Goa LD, Lu GC, Weo RL.
Intraocular lowering effects of commonly used fixed-combination drugs with
timolol. A Systemic Review and Meta-Analysis. PLoS One 2012; 7 (9): e4 5079.
3.
Lee AJ, Rochtchina E, Wang JJ,
Schneider J.
Does smoking effects intraocular pressure, findings of Blue Mountains Study. J
Glaucoma. 2003; 12: 212.
4.
Chihara E. Assessment of
true intraocular pressure: the gap between theory and practical data, Surv
Ophthalmol 2008; 53 (3): 203-18.
5.
Almubrad TM, Ogbuehi KC. The effect of
repeated applanation on subsequent IOP measurements. Clin Exp Optom 2008; 91: 524-9.
6.
Salim S, Linn DJ, Echols JR, Netland
PA.
Comparison of Intraocular pressure measurement with the portable PT-100
non-contact Tonometer and Goldmann Applanation tonometry. Clin Ophthalmol.
2009; 3: 342-4
7.
Yaoeda K, Shirakashi M, Fukushima A,
Funaki S, Funaki H, Ofuchi N, Nakatsue T, Abe H. Measurement of intraocular pressure
using the NT-4000: a new non-contact tonometer equipped with pulse synchronous
measurement function. J Glaucoma. 2005; 14: 201-5.
8.
Tonnu PA, Ho T, Sharma K, White E,
Bunce C, Garway-Heath D. A comparison of four methods of tonometry: method agreement and
interobserver variability. Br J Ophthalmol. 2005; 89: 847-50.